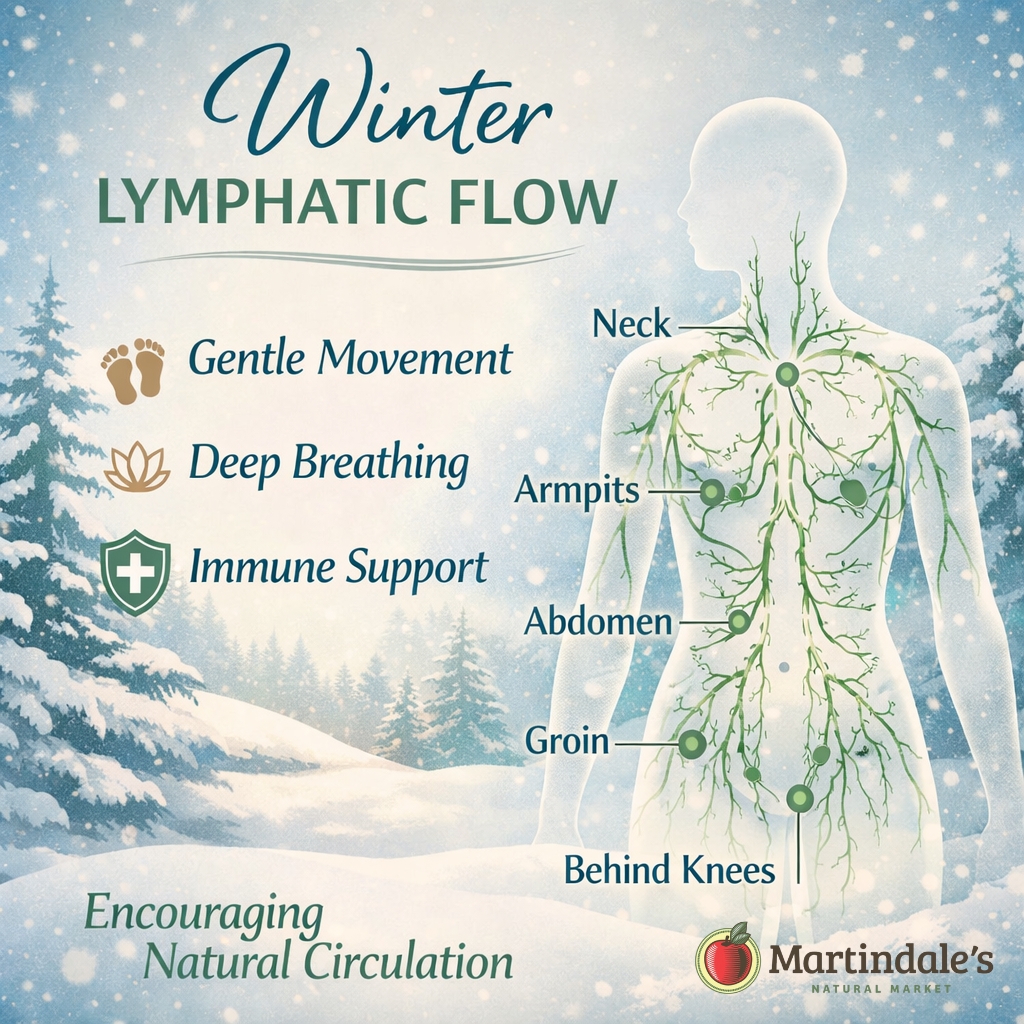
Winter Lymphatic Flow
Seasonal Lymphatic Health
Lymphatic Flow and Immune Communication
Why Puffiness and Heaviness Increase in Winter
- Decreased physical movement
- Slower circulation
- More time spent sitting.
Breathing and the Lymphatic System
Lymphatic Health Is a Lifestyle
Scientific understanding shows that:
-
The liver is a primary site of biotransformation (detoxification) that helps process substances so they can be eliminated (NCBI Bookshelf explains liver detoxification/processing functions in plain language) — How the liver works (NCBI Bookshelf)
-
The kidneys play a major role in eliminating unwanted substances—including drugs and metabolites—through filtration and secretion (NCBI Bookshelf overview of renal physiology and tubular secretion) — Physiology, Renal (NCBI Bookshelf)
-
The lymphatic system supports fluid balance and immune transport (NCI definition notes its role in fluid levels and immune system support) — Lymphatic system definition (National Cancer Institute)
-
Daily movement is a key driver of lymph transport, and periods of inactivity can reduce lymph flow efficiency (NIH PubMed Central review on lymphatic pumping/transport).
-
Poor sleep and chronic stress can disrupt immune regulation (which matters because lymphatic tissues are central to immune communication) — Sleep and immune function (NIH PubMed Central)
Herbs Traditionally Used for Lymphatic Support
In traditional and alternative herbal systems, certain roots and botanicals were selected for their relationship to fluid movement, tissue health, and overall balance. These herbs were not used to “force detoxification,” but rather to support the body’s natural processes gently and over time, alongside daily movement, hydration, nourishment, and rest.
In Western herbal traditions—especially the Eclectic and Physiomedical systems that developed in 19th-century America—practitioners viewed the body as an interconnected whole. These traditions emphasized plant-based remedies, careful observation, and support for circulation, tissue tone, and natural balance over time. Rather than targeting a single system in isolation, practitioners combined herbs to work gently alongside the body’s own processes. Traditional Chinese Medicine follows a similar whole-system approach.
Below are three herbs frequently referenced in historical herbal literature in relation to lymphatic support.
Echinacea angustifolia (Root)
Echinacea root has a long history of use in Western herbalism, especially within Eclectic medical traditions of the 19th and early 20th centuries. Herbalists traditionally worked with echinacea root to support tissue tone and overall systemic balance, particularly during times when the body was under stress.
The National Center for Complementary and Integrative Health (NCCIH) summarizes echinacea’s traditional use and historical context within herbal medicine.
👉 https://www.nccih.nih.gov/health/echinacea
Red Root (Ceanothus americanus)
Historical herbal literature frequently references red root when discussing lymphatic support. Eclectic and Physiomedical practitioners—two historical schools of American herbal medicine—studied plant remedies alongside anatomy and physiology. They described red root in relation to sluggish lymph movement and tissue congestion. These patterns often appeared during seasonal changes or in certain constitutional types.
👉 https://www.henriettes-herb.com/eclectic/kings/ceanothus.html
These texts reflect how herbalists historically understood and applied red root within broader wellness formulas.
Burdock Root (Arctium lappa)
Western herbalism and Traditional Chinese Medicine have used burdock root for centuries. Herbal practitioners valued it as a gentle, long-term herb. They associated it with supporting tissue health, fluid movement, and overall balanc
For example, traditional herbal texts and modern herbal education sources describe burdock root as an herb that supports the body’s filtration and transport systems, including pathways historically associated with lymphatic flow and the movement of wastes out of tissues. This traditional understanding is outlined by The Herbal Academy, a respected herbal education organization that documents burdock’s role in traditional lymphatic and alterative herbal practice.
👉 https://theherbalacademy.com/blog/creating-local-materia-medica-burdock/
How These Herbs Were Traditionally Used Together
In traditional practice, these herbs were rarely used alone. Herbalists historically combined plants with complementary actions into balanced formulas. These blends focused on supporting fluid balance, tissue health, and natural circulation. They worked gently over time. Herbalists also paired them with daily habits like movement, hydration, nourishment, and rest.
For example, classical herbalists grouped herbs such as burdock root, red root, echinacea, cleavers, and red clover into alterative or tonic formulas. These formulas supported the body’s natural elimination pathways, including the lymphatic system. Herbalists viewed alterative herbs as tools for restoring overall balance. They used these herbs to support lymphatic circulation, organ elimination, and tissue health. These effects were strongest when herbs were combined thoughtfully rather than used on their own.
Today, this traditional approach is sometimes referred to as “lymphatic detox.” From a historical perspective, it is more accurately described as gentle lymphatic support rooted in long-standing herbal traditions.
The “Big 6” Gentle Lymph Areas
- Neck (Cervical Area) – Supports drainage from the head and face.
- Above the Collarbone (Supraclavicular Area) – A major lymphatic exit pathway
- Under the Arms (Axillary Area) – Drains the arms and upper torso.
- Abdomen – Supports digestive and immune lymph flow.
- Groin (Inguinal Area) – Drains the lower body.
- Behind the Knees (Popliteal Area) – Supports lymph flow from the legs and feet.
A Winter Wellness Perspective
These statements have not been evaluated by the FDA. They are not intended to treat, diagnose, cure or prevent any disease.
